Infectious Disease Update: A Tale of Three Rashes
Sheila Fallon-Friedlander, MD
Molluscum Contagiosum (MC)
Molluscum contagiosum usually occurs in children 0-14 years of age; however, Dr Friedlander reminds us that it can be seen in adults and transmitted sexually. The highest incidence occurs in children one to four years of age. There are definite associations that we need to keep in mind, i.e, swimming and eczema both appear to be associated with either a higher risk of getting the disease or a more prolonged course.
Unfortunately, there is a subset of patients may have a more prolonged or severe course.
Families often want to know exactly how long it has been incubating and how long it will be there. Incubation is normally two to eight weeks. Molluscum infections can persist for years in some unlikely children, with an average duration of eight months. Generally, molluscum is asymptomatic; however, patients may be bothered with pruritus, erythema, bacterial superinfections, inflammation and pain.
What are the troublesome cutaneous findings associated with MC?
Atopy is prevalent in 44 percent of kids who present with MC (AD, asthma or allergies). What might be troublesome for you is the child who comes in with molluscum dermatitis, as this can occur in up to 39 percent of patients. The biggest problem is the patient with inflamed lesions as everyone thinks the child is infected and you need to take action. In one study, this occurred in 22 percent of patients. Another significant associated rash that we have seen is Gianotti-Crosti Syndrome-like reactions where you will see lichenoid papules around the elbows, knees, and buttocks. In children, if you note Gianotti-Crosti, type eruptions, think associated viral infections. Though we have traditionally been trained to think of EBV or hepatitis, Dr Friedlander suggests that you look to see if they have molluscum because many of them will.
What is BOTE?
BOTE is the “Beginning Of The End”, i.e., a predictor of resolution of the molluscum infection. Remember that the inflammatory phase of molluscum infection includes MC dermatitis, extreme induration and erythema, fluctuance, purulent exudate, “pseudo abcesses” and “ pseudo furuncles.” The onset of this type of inflammation to disease resolution is thought to be from three weeks to five months. (Butala N, et al. Pediatric. 2013;131:e1650.)
Why is it important to recognize “BOTE”?
The recognition of BOTE helps to avoid unnecessary cultures, antibiotics, admissions and the development of antibiotic resistance. Findings that should raise concern are a cellulitis-like appearance and lymphangitic streaking. If the child looks sick or is running fevers, you need to take action; however, if a child looks perfectly well, has multiple spots that have been red and inflamed looking for a while, and there’s no lymphangitic streaking, then you should keep BOTE in mind.
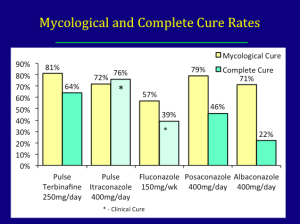
Treatment
What do the scientists tell us? Why is it so hard to clear? MC expresses proteins that circumvent immune responses (FLIPs) that inhibit b-interferon activation. What is Dr Friedlander’s hands down favorite therapy for molluscum? Cantheridin 0.7% in collodion applied with a Q-tip, washed off in four-to six hours. Some families are very nervous with this, so you can do test sites. Be sure to warn the family about the occurrence of blisters. What are the No-Nos? Catherone Plus for molluscum-NO. Do not do anything other than topical retinoids to the face , and intertriginous areas can develop severe blistering eroded reactions.
Cantharidin is an excellent treatment for molluscum but usually needs to be purchased from Canada or a compounded pharmacy. It can be ordered online through ABC pharmacy.com (Canthardin 7.5ml ~ $100.00) For those who have a willing hospital pharmacy, crystals can be ordered from Gallipot. The Cantharidin crystals themselves cost approximately $192.00/gm; when compounded it comes to $45.00/bottle.
Why don’t we let patients take Cantharidin home?
Topical application of Cantharidin for an extended time, extended areas or under occlusion and oral ingestion may cause serious side effects such as lymphangitis, TSS, and fatal poisoning. Beware of applying Cantharidin to intertriginous sites.
Another Option—The George Martin Method
- Obtain monochloracetic acid
- Fill small clean biopsy container half-way with crystals
- Add water half-way (saturated solution)
- Apply a very small amount with a toothpick
- Neutralize in 60 seconds with a wet paper towel
Patients can expect crusting and blistering in about two weeks.
Clinical Pearl—Remember the BOTE sign—avoid needless interventions in your molluscum patients
What do you need to think about when you see a purpuric rash?
You need to consider infection, i.e., bacterial, or viral. Also think about decreased production of marrow cells due to drug reaction, leukemia, or myeloproliferative disorders. Is there an increased consumption of marrow cells due to drug, ITP, hemolytic disorders or parvovirus? Let all of these possibilities run through your mind.
If you see lesions on the foot and hands, you may consider “hand, foot, and mouth disease” and Coxsackie. Usually Coxsackie virus is caused by A16. The disease usually occurs in spring-autumn in temperate climates and affects kids less than one to five years old. Most infections are asymptomatic. Patients may present with ulcerative stomatitis, lesions on the palms and soles and sometimes on the knees, elbows, buttocks, and genitals.
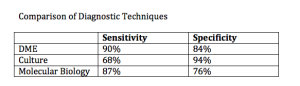
Coxsackie A6
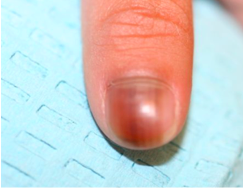
Coxsackie 6 was first noted in 2011 by the CDC. How does it differ from regular Coxsackie? There is a wider age range with this disease. There may be vesiculobullous lesions present that are giant and a large area of involvement. There may be a rash that looks severe, but children tend not to look as sick. The problem with this disease is that if you were to try to culture it, it does not grow well in cultures. PCR however can nail it if it is available. You have to have clinical suspicion. What may help you nail the diagnosis if you don’t have PCR? Look at the mother’s nails. And if a child comes in with nail shedding, think Coxsackie. Dr Friedlander’s practice saw several cases of onychomadesis in the office; when the moms were asked they mentioned that the children were sick about a month prior. Your first presentation of Coxsackie in the office may be a child whose nails are shedding or a mother’s.
What do we do with this child? We look at him/her, we look at the overall health of the child and we make sure that it isn’t something serious by clinical evaluation. When in doubt, evaluate for other more serious possibilities. With Coxsackie disease, we can reassure.
Look What the Wind Blew In…
A patient presents with a prolonged fever and a polymorphous eruption that looks a bit like erythema multiforme, a little bit like morbilliform, even measles-like. You need to think about bacterial and viral infections and you need to think about drug. You look at his conjunctivae and you notice limbal sparing, an area of white that is different from what you would get with adenovirus or Steven’s Johnson syndrome. When you undress the child, you notice a very distinctive perineal desquamating rash. This is Kawasaki’s Disease. You need to recognize this because while you may not see this often, when you do, you can save a life.
Kawasaki Disease (KD)
KD is a small- and medium-size artery vasculitis. There is now evidence that the incidence of KD may be linked to the velocity and direction of wind currents.
The typical age at presentation is six months to five years of age. The highest incidence of the disease is in Asian countries, and in the United States the incidence of KD is highest among the Asian population. If a child has KD, his/her siblings are six-to 30 times more at risk than the normal population and if a person had KD as a child, his/her child as a two time greater risk of the disease. The recurrence rate for the disease is two to four percent.
KD characteristics include a fever for more than five days as well as a rash that is variable but does not blister , and conjunctivitis (non exudative, non-limbal). KD affects the lips and tongue and there may be cervical lymphadenopathy as well as erythema/edema of the palms and soles as well as desquamation.
It is imperative that you intervene quickly with KD as this can decrease coronary risk by at least a factor of five.
Summary
With regards to pediatric infectious diseases, it is imperative that you know when to reassure, when to prevent unnecessary interventions and know when to act quickly!