Atopic Dermatitis: Epidemiology & Beyond
By Jonathan I. Silverberg, MD, PhD, MPH
The global prevalence of atopic dermatitis (AD) has been estimated at about 15% to 20% in pediatric and 1% to 10% of adult populations. The prevalence has increased in the past few decades in many regions.
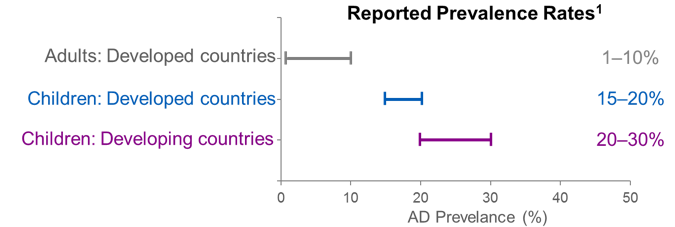
Figure 1. Reported prevalence rates of AD vary between adults and children and, for pediatric patients, are higher in developing nations than the industrialized world
It was thought that AD prevalence has increased primarily in the developed world, but it is not possible to draw clear lines of demarcation.1 Sometimes national variations can be striking and seem to defy explanation.
For example, among pediatric patients in the age range of 6 to 7 years, the prevalence of AD was, from lowest to highest, 0.9% in India and 22.5% in Ecuador.2 Among older children (aged 13 to 14), prevalence was lower in China, Asia-Pacific, the Middle East, India, and parts of Latin America but higher in some parts of Africa, Northern and Eastern Europe, and Oceania.2 The prevalence rates for AD vary broadly by developed versus developing nation and are higher for children than adults, see Figure 1.
Factors that may help to explain the global variations in AD prevalence:
- Genetic factors
- Environmental factors
- Microbial exposures
- Immune dysfunction
- Definitions of AD, eczema, diagnostic criteria3
Most cases of childhood AD start in in the first five years of life. Approximately, 20-50% of childhood AD persists into adulthood.4 However, adult onset AD is quite common, with one in four adults with AD report adult-onset of their disease.5
Emerging data suggest that family structure may play a role in AD rates. Using multivariable logistic regression and adjusting for socio-demographic factors, it was found that US children from single-adult households, families with a mother but no father present, families with unmarried mothers, and families with non-biological fathers had increased odds of developing AD.6 Other risk factors for AD include cigarette smoking and exposure to second-hand smoke.7 Moreover, both adults and children with AD have higher rates of mental health symptoms, such as depression and anxiety.8,9
AD is characterized by a dysregulation of the immune system and a disruption in the skin’s barrier function. These conditions may set the stage for AD-associated comorbidities. Some of these comorbidities may be interrelated and their exact association with AD may not be yet entirely elucidated.10
- Cutaneous infections, including extra-cutaneous infections (such as sepsis)
- Disturbed sleep, sleep inefficiency, fatigue
- Cardiovascular conditions, such as atherosclerosis, myocardial infarction, congestive heart failure
- Cerebrovascular disorders, including stroke
- Obesity
- Hypertension
- Hyperlipidemia
- Diabetes type II
The burden of AD is not trivial. Patients experience severe and sometimes relentless pruritus, may have skin pain11 experience sleep and mental health disturbances, and suffer from an unsightly rash that may cause embarrassment and social isolation. Most AD patients (88%) report the daily presence of itchy skin and 69% report that the itchiness lasts at least 12 hours a day. Fifty percent of AD patients report pain accompanies pruritus and 69% describe the itchiness as being severe or unbearable. Most AD patients (90%) report that their AD disrupts sleep at least one night per week.12-14
AD is a highly prevalent condition associated with serious comorbidities, a high disease burden, and great costs to the healthcare system.
References
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Annals of nutrition & metabolism. 2015;66 Suppl 1:8-16.
- Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI. Global variations in prevalence of eczema symptoms in children from ISAAC Phase Three. The journal of allergy and clinical immunology. 2009;124(6):1251-1258.e1223.
- Dizon MP, Yu AM, Singh RK, et al. Systematic review of atopic dermatitis disease definition in studies using routinely collected health data. The British journal of dermatology. 2018;178(6):1280-1287.
- Kim JP, Chao LX, Simpson EL, Silverberg JI. Persistence of atopic dermatitis (AD): A systematic review and meta-analysis Journal of the American Academy of Dermatology, Vol. 75, Issue 4, p681–687.e11. Published online: August 18, 2016
- Lee HH, Patel KR, Singam V, et al. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis. Journal of the American Academy of Dermatology. Published online: June 1, 2018
- McKenzie C, Silverberg JI. Association of family structure with atopic dermatitis in United States children. Journal of the American Academy of Dermatology. 2018.
- Kantor R, Dalal P, Cella D, Silverberg JI. Research letter: Impact of pruritus on quality of life—A systematic review. Journal of the American Academy of Dermatology, Vol. 75, Issue 5, p885–886.e4. Published online: August 28, 2016
- Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. The Journal of allergy and clinical immunology. 2013;131(2):428-433.
- Yu SH, Silverberg JI. Association between Atopic Dermatitis and Depression in US Adults. The Journal of investigative dermatology. 2015;135(12):3183-3186.
- Silverberg JI. Associations between atopic dermatitis and other disorders. F1000Research. 2018;7:303.
- Vakharia PP, Chopra R, Sacotte R, et al. Burden of skin pain in atopic dermatitis Annals of Allergy, Asthma & Immunology, Vol. 119, Issue 6, p548–552.e3. Published in issue: December 2017
- Simpson EL, Bieber T, Eckert L, et al. Patient burden of moderate to severe atopic dermatitis (AD): Insights from a phase 2b clinical trial of dupilumab in adults. Journal of the American Academy of Dermatology. 2016;74(3):491-498.
- Dawn A, Papoiu AD, Chan YH, Rapp SR, Rassette N, Yosipovitch G. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. The British journal of dermatology. 2009;160(3):642-644.
- O’Neill JL, Chan YH, Rapp SR, Yosipovitch G. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta dermato-venereologica. 2011;91(5):537-540.

