Malpractice and Informed Consent
Mathew M. Avram, MD, JD
One of the keys to a happy patient is to set realistic expectations and to obtain an appropriate informed consent. Dr Avram, a world-renowned cosmetic surgeon and former practicing attorney, provides us with some important basic information and key concepts that can help us navigate some potentially confusing legal issues.
There are four required elements to a malpractice suit:
- Breach
- Of a duty
- That causes
- Harm
Duty
The standard is that of a “reasonable duty.” This is the quality of care at a level consonant with medical knowledge and judgment that a physician is reasonably expected to posses. When that standard is litigated, there are a couple of different ways that this can be done, e.g., expert testimony, medical literature, standard practice, and clinical guidelines. When using expert witness qualifications, remember that the expert must have sufficient training to assess the physician’s performance. Keep in mind; however, that this is ultimately at the trial judge’s discretion and there is no requirement for board certification.
The plaintiff’s expert testimony must establish a standard of care and must be able to establish that the physician failed to meet that standard to a “reasonable degree of medical and scientific certainty.”
Negligence can also be established through:
- Cross examination of defendant’s expert witness
- FDA/PDR warnings
- Learned treatise
- Defendant admission of negligence—“Sorry, I hurt you. Don’t worry, I have insurance.”
Defenses to a Malpractice Suit
Respectable Minority Exception
This is where there are two (or more) schools of thought as to a procedure and a physician can pursue one of many treatment options that a “considerate number of reputable and respected physicians” pursue. (E.g. cryotherapy versus topicals for AKs)
Contributory Fault
This is where a patient makes mistakes or certain lifestyle choices. Damages to the plaintiff are mitigated by failure to exercise ordinary care, i.e., drinking alcohol while taking terbinafine.
Statute of Limitations
These are usually two to three years after injury or malpractice. The key is the timing, i.e., the timing from when the defendant breaches his/her duty or when the plaintiff suffers injury. What can make this complicated is when the plaintiff becomes aware or reasonably should be aware of the injury. (e.g., delayed hypopigmentation six months after CO2 resurfacing or granuloma years after a permanent filler treatment) Depending on the procedure and its consequences, the statute of limitations can be extended.
Doctrine of Informed Consent
Remember that your informed consents are NOT going to protect you against a malpractice case and vice versa. These are two distinct legal theories by which you can be sued.
All patients have the right to an informed consent prior to any treatment.
Failure to obtain an informed consent constitutes a battery and the physician is liable for civil damages. Consent can be written or oral.
As a physician, you need to examine the probability of risk and the severity of the side effect. Thus even the small chance of blindness with soft tissue filler injections needs to be included in your consent forms. You also need to examine particular susceptibilities of the patient, i.e., hyperpigmentation in a patient with a darker skin type undergoing laser procedure. Your duty becomes expanded as the patient asks more questions.
In terms of your consents, keep it simple. A written consent is ineffective if the patient doesn’t understand material information about the procedure. Avoid technical medical terms and use lay person terms.
Purpura–Bruising
Erythema–Redness
Standards of Disclosure-The patient must have the capacity to make a medical decision. Remember that minors lack this capacity and parents must consent to all medical or cosmetic procedures.
Blanket Authorizations-Overbroad written consents are viewed by disfavor by courts, they like more specificity to show an informed consent.
If a patient misleads a physician, this can be defense to an informed consent action. The patient has a duty to disclose accurate information. Regarding patient decision making limitations, absent of showing incompetence, the courts presume patient comprehension.
Tips to Avoid a Law Suit
Patient selection is a key decision. Assess the patient the patient at consultation, particularly their expectations. Trust your own intuition about a patient as well as your staff’s intuition. For elective, cosmetic treatments, don’t be afraid to say NO.
Studies have shown that your relationship with the patient may be the single most important factor in avoiding a lawsuit. Patients with a good relationship with their physician are far less likely sue.
Avoiding Complications
Know your limits—even in skilled hands, if you treat a sufficient number of patients, you will encounter challenging side effects. Do not perform a procedure that might produce a single side effect that you cannot recognize and treat. Remember the complications are inevitable; however, good practice and common sense can minimize complications significantly. Do not abandon or avoid a patient with a poor outcome or side effect. This is bad medicine and rightfully angers your patients increasing your risk of a lawsuit.
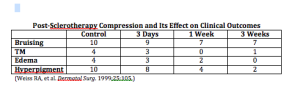
If you are uncertain as to what is happening, you should consult with a colleague. Temporary and expected side effects are common. These include erythema, edema, and purpura. Legal consequences are less likely with adequate patient handholding.
Regarding botulinum toxins, litigation for cosmetic treatments is rare and less common than for lasers. With lasers we may see temporary pigmentation, but time is on your side and the discoloration will most likely resolve before any litigation proceeds.
More permanent side effects are more likely to produce liability (e.g. scars, blindness). It is important to distinguish how long-term these side effects actually are.
Documentation
Documentation is crucial. Document physical findings on the exam, even the ones that aren’t necessarily related to what’s happening. Good photography is important because poor photography will work against you. Also ensure that your consent forms are properly filled out.
Lasers and Lawsuits
A study by Dr Avram and his colleagues published in JAMA dermatology looked to identify common errors/risk factors for litigation in laser surgery through a search of an online legal research database. They reviewed over 1600 documents that were retrieved by their search criteria and found 182 unique legal claims involving injury from a cutaneous laser treatment. Not surprisingly, New York, California and Texas were the most common areas, given their populations. The most common litigated procedures were hair removal, rejuvenation (mostly IPL), and vascular treatments. The most common injuries sustained were burn, scar and pigmentation. The most common causes of action were standard of care, informed consent, and fraud (exaggeration of benefits).
Non-Physician Litigation Data
From 2008 to 2011, there has been a dramatic increase in litigation against non-physician operators. In 2008, non-physician laser treatments and litigation represented 36.3 percent of all laser-related cases whereas in 2011 it represented 77.8 percent of cases. Only 23.4 percent of non-physician operation litigation cases arose in medical office settings. 76.6 percent of the cases were performed outside a traditional medical setting such as salons and spas (mainly laser hair removal). The majority of these cases were performed without any direct physician supervision.
Physician Extenders
The physician is held liable for a physician extender’s negligence provided that he/she is an employee receiving a salary, benefits and performing within his/her scope of duty. This is regardless of whether or not the physician saw the patient at the time of the visit. Supervision of non-physician laser procedures varies from state to state. Some jurisdictions require on-site supervision by physicians, while others do not.