Rosacea
Richard Gallo, MD, PhD
In this presentation at MauiDerm 2014, Dr Richard Gallo, an expert in the field, provides us with an update on the management of rosacea…
Remember that rosacea almost exclusively affects the face, making it both a cosmetic and medical issue for those it affects. For the clinician, rosacea is a prevalent, serious, recurring and progressive dermatological condition that requires chronic therapy to prevent long-term sequelae. Rosacea affects approximately 14 million Americans and possibly more. Unfortunately, the condition is often times not recognized; however, we have found that early recognition and treatment are important in order to prevent progression and disfigurement. Therapeutic regimens must be tailored to the individual patients and need to address acute symptoms, help patients remain asymptomatic, and minimize the recurrence of symptoms.
Rosacea can be categorized into four sub-types: subtype 1-erythematotelangiectatic; subtype 2-papulopustular; subtype 3-phymatous; and subtype 4-ocular. (Wilkin J, et al. J Am Acad Derm 2002;46:584-587; Wilkin J, et al. J Am Acad Derm. 2004;50:907-912.) There are also many different variants of this disorder that do not always clearly fit into the above-mentioned subtypes such as vascular, sebaceous hyperplasia/rhinophyma and inflammatory causes.
The diagnosis of rosacea is based upon consensus opinions. We don’t have a clinical test or laboratory value, i.e., some sort of objective measurement that can determine rosacea.
Primary Diagnostic Features of Rosacea
- Central facial erythema (fixed)
- Flushing
- Telangiectasias
- +/- inflammatory lesions
Secondary Diagnostic Features
- Burning or stinging
- Plaque
- Dry appearance and scale
- Edema
- Ocular manifestations
- Peripheral location
- Phymatous changes
(Del Rosso, J.Q., Thiboutot, D., Gallo, R.L. et al. Consensus Recommendations from the American Acne & Rosacea Society on the Management of Rosacea, Part 1. Cutis 2013; 234-240;
Wilkin, J, Dahl, M, Detmar, M, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002; 46:584.)
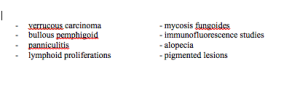
Unfortunately, rosacea is often misdiagnosed. Rosacea is variable in that there are various combinations of cutaneous signs, such as flushing, erythema, telangiectasia, edema, papules, pustules, ocular lesions and rhinophyma. Diagnostic confusion can occur because most patients only have some, rather than all, of these signs and symptoms. Other dermatological disorders and co-morbid conditions affecting the face can also cause confusion. Rosacea is often confused with acne and it may coincide with actinic keratosis, acne, seborrheic dermatitis, and contact dermatitis.
Inflammation is a major culprit! Inflammation in rosacea may result in capillary cell wall weakening secondary to dermal-matrix deterioration. It may also result in lymphatic failure secondary to elastin degradation and/or the production of vascular mediators. Inflammation precipitates episodic signs and symptoms of rosacea.
In order to really understand this disease, we need to understand the origin of inflammation. To come up with a way to effectively treat our patients we need to understand what causes this disease.
There are several environmental exposures that can trigger rosacea:
(Patient reported survey in rank order)
- Sun exposure
- Emotional stress
- Hot weather
- Wind
- Heavy exercise
- Alcohol consumption
- Hot baths
- Cold weather
- Spicy foods
- Humidity
- Indoor heat
- Certain skin-care products
- Heated beverages
- Certain cosmetics
- Medications
- Medical conditions
- Certain fruits
- Marinated meats
- Certain vegetables
- Dairy products
Can all of the subtypes and all of the different triggers really be the same disease?
Normal facial skin uses pattern recognition molecules to detect danger. Toll-like receptors are just one of many types of molecules that exist on the surface of keratinocytes and every cell type of the skin. Their goal is to detect patterns of the environment around them. Multiple microbes, dry skin and UV are all triggers of the pattern recognition system. Researchers began looking at biopsies of rosacea patients on non-inflamed skin. One particular concept was that rosacea patients have too much PRR (pattern recognition receptor) activity as seen by TLR2 protein staining. This is an important issue to understand as it explains the essential role of general skin care as the skin has an excess of the molecular sensors of damage. UV injury as well as excessive dryness and even excessive oilyness triggers PRRs. This idea helps to put other theories into context.
Theories About Triggers
O’Reilly and colleagues published a paper demonstrating the positive correlation between serum immunoreactivity to Demodex-associated Bacillus proteins and erythematotelaniectatic rosacea. Eighty percent (21/26) of patients with erythematotelangiectatic rosacea showed serum reactivity to B. oleronius, compared with forty percent (9/2) of controls. (O’Reilly N, et al. Br J Dermatol. 2012) However, there are problems with this hypothesis. First of all this is fairly rare, one mite out of forty contained the bug and cross-reactivity of the bug antigens with other more common bugs has not yet been investigated. Many normal patients have this bug and did not react to it. Lastly, trying to kill Demodex is not usually effective for patients with rosacea. The take home message for current trigger data is that we, as clinicians, need to care for the barrier and remember that there is probably no single trigger for everyone. This makes patient history, clinical exam and your relationship with patients incredibly important.
What do the triggers do?
LL-37 expression is increased in rosacea. LL-37 is a very important molecule in a number of skin diseases in that it kills microbes as well as increases vasculature and inflammation upon its release. The other part of the equation that is important is the molecule KLK5, which is an enzyme that activates LL-37. So when we think about rosacea, remember that there are various signals that are activated by the environmental triggers. This is variable based on genetic makeup and the ecological organisms on the skin. A normal innate immune system reacts to infection and true danger, there is no inflammation in a resting state. Rosacea patients; however, have a molecular sensitive skin because of too much PRR. Once that is triggered, the trigger system makes too much KLK5 that can activate LL-37 and initiate certain aspects of this disease.
It is important to understand the role of KLK and LL37 in rosacea because they explain the benefits of current therapies. They may also serve as a potential objective biomarker as well as aiding in future new drug development. Dr Gallo and many others have worked in larger studies to validate and confirm these observations. A blinded study conducted by Coda and colleagues looked at the KLK enzyme on the skin and found that rosacea patients have elevated enzyme activity but divide into two populations that weren’t necessarily distinguishable on clinical presentation. This may be important because protease level can predict topical azeleic acid response. Patients with high enzyme activity who were treated with azeleic acid showed a significant drop in activity over sixteen weeks, whereas patients who started off with low protease activity showed no response. (Coda, et al. JAAD. 2013)
Other therapies that we currently have may also be working because of a similar process. The tetracycline class drugs have shown to inhibit this enzyme. When we look back at old literature, we see that some of the biochemists found that one of the things that tetracycline seemed to do was inhibit enzyme activity completely independent of any action on a bacteria.
Testing the Hypothesis: Does targeted inhibition of KLK5 activity improve rosacea?
Dr Gallo and colleagues conducted a pilot clinical trial using an FDA-approved serine protease inhibitor that was formulated into a topical cream. It was a 12-week, double-blind, placebo controlled BID application to measure both protease and clinical response. The only patients who improved in this trial were those who applied the protease inhibitor. (Two, A.M. et al. J Invest Dermatol. 2013) This is not necessarily proof of a new therapy, but it is intriguing data that may prove the theory relevant.
In summary, rosacea patients have high KLK5 and LL37. KLK5 activates cathelicidin and more LL-37 and KLK5 is associated with disease severity. Successful therapies are associated with decreased KLK5 activity or cathelicidin.
Neuromediators Are Important!
Neuromediators increase vasodilatation, nerve endings, neuropeptides and they stimulate mast cells. What can we do about this? We have alternative neuromediators that fight these vasodilitation effects. The alpha-adrenoceptor agonists are the stimuli are the alpha1 and alpha2 receptors. They have the ability to initiate smooth muscle contraction in a dilated vessel. When topically applied, both brimonidine (a2 agonist) and oxymetazoline (a1 agonist and a2 agonist) have shown to be successful therapies for the erythematous stage of rosacea. (Fowler J et al. J Drugs Dermatol. 2013; Shanler and Ondo Arch Derm 2007) These are alternative mechanisms thinking about the pathology of the disease. The drivers of the disease are the molecules that initiate inflammation and vascular growth. We now have strategies for inhibiting or reducing LL-37 and limiting vasoactive response.
Topical Rosacea Therapy
The goal of topical therapy is barrier repair, decrease triggers, decrease LL-37 and vasoconstriction. Don’t forget to always include appropriate barrier care such as sunscreen, gentle cleansers and moisturizers.
- Azeleic acid
- Sodium sulfacetamide/sulfur
- Brimonidine
- Metronidazole
- Tretinoin
- Tacrolimus/pimecrolimus
- BP/Clinda
- Ivermectin
Oral Rosacea Therapy
Oral therapy targets triggers and drivers.
- Tetra/doxy/mino
- Cipro
- Bactrim
- Isotretinoin
Clinical Pearls
Early Rosacea
- Trying to minimize triggers
- Rosacea drivers not major yet
- Complaint is erythema
What should we do?
- Trigger avoidance
- Barrier care
- Topical agent
- Adrenergic agonist
Moderate/severe Papulopustular
- Still need to minimize triggers
- Rosacea drivers active
- Complaint is red papules
What should we do?
- Oral agent (TCN)
- Barrier care ±sunscreen
- Topical agent
- Adrenergic agonist
- Second line Isotretinoin
Perioral Rosacea
- Spared vermillion
- Microbial influence?
- Ask about steroid
What should we do?
- Oral agent (TCN)
- Barrier care
- Possible TIM
In conclusion, we are finally getting a mechanistic understanding of rosacea. There is a need for an individual approach and both rosacea triggers and drivers need to be identified and targeted. We have good and complementary options for medical therapy. Do not forget the importance of barrier care!!
MauiDerm News Editor-Judy Seraphine