Jerry Shapiro, MD
Dr Shapiro, an expert in hair loss treatment, provided the audience with a practical approach to treating hair loss. Dr Shapiro practices in Vancouver, Canada and New York, New York. In Canada, he sees 60-70 patients per day and 70 percent of his patients are female. 35 percent are PHL and telogen effluvium, 30 percent are alopecia areata, and 35 percent are cicatricial alopecias.
Hair Loss in Women: Part 1
It’s important to know that at least one third of women experience hair loss and the effect of hair loss on patients’ emotions is often greatly underestimated by physicians. As a clinician, you almost need to act as a detective to find out the cause of the hair loss. It is imperative that you spend a good amount of time talking to your patients about their hair loss, trying to assess an approximate duration of time since their hair loss began. Of note, the youngest cases of MPHL and FPHL that Dr Shapiro has seen is age eight and it happens suddenly versus gradually. Ask your patients whether or not their hair loss was sudden or gradual. Another important step in evaluating hair loss is to assess the pattern. We should all be familiar with the Ludwig classification of Female Pattern Hair Loss ranging from classes I to III. Also of importance is to address whether the hair loss is thinning or shedding. The key question for shedding is to ask “is there hair on your pillow?” and “is there hair in your food? or on the stove? Is there hair in the fridge?” Keep in mind that you need to lose 50 percent of scalp hair to notice any change clinically. So, someone who has 100,000 hairs and someone who has 50,000 hairs look exactly the same, you can’t necessarily see that clinically.
The next step in the evaluation is to determine whether the hair is falling out from the roots or whether it is breaking. Hair loss from the roots can be associated with AGA, telogen effluvium, or alopecia areata; hair breaking with tinea capitis, cosmetics/trichotillomania, or hair shaft abnormalities. A thorough evaluation also includes taking a good family history. Remember that family history includes siblings, aunts, uncles, and grandparents—not just the mother and the father. Hair care practices are also very important, i.e., how often do they go to the hair dresser, how often do they shampoo, what products do they apply to their scalp? There are sorts of hair care practices that can cause hair loss.
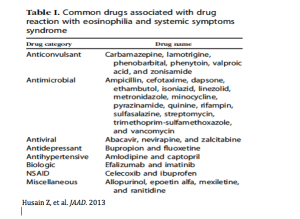
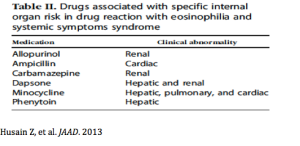
When talking to your female patients, you need to address any systemic illnesses, recent childbirth, recent surgery and any psychosocial stressors. Psychosocial stressors such as bereavement, break-up/divorce, and bankruptcy can initiate a telogen effluvium. New medications can initiate hair loss within one to three months. (Some of these medications include acetretin, heparin, interferon alfa, isotretinoin, ramipril, and many more.)
Factors that might indicate androgen excess and thus can contribute to hair loss include seborrheic dermatitis, acne, hirsutism, and irregular menstrual cycles. Other important questions include signs of hypo or hyperthyroidism, heavy menstruation, and a vegetarian diet.
Five Stages of the Clinical Evaluation
- Distribution of hair loss—where is it on the scalp? We tend to think that this is just on the top, but that’s not the case.
- Inflammation, scale and erythema
- Scarring vs. non-scarring—you may have to use your dermatoscope in order to see the ostia.
- Quality of hair shaft—determine how much they have grown and whether or not the hairs are broken. Are there new hairs growing in? This can tell you whether or not the treatment is working…patients like to hear that there is regrowth.
- Pull test—tug at 60 hours in order to see how many hairs you can get. Make sure that patients have not shampooed that day because the results can give you a false negative.
Diagnostic Tools
There are several new diagnostic tools available for the scalp and these include dermascopy (10-fold magnification), videodermascopy (50-100-fold magnification), and folliscope that magnifies the scalp 50-100 times. This can count how many hairs the patient has per square centimeter and determine how wide the hairs are. It will tell you how many microns each individual hair is and give you an average at the end. Patients really appreciate this, they see you do this in front of them and they feel that you are doing something very useful. Dr Shapiro feels that because of this, he has been able to reduce the number of biopsies because he can now make a diagnosis frequently using trichoscopy or the folliscope. Usually you want your hairs more than 60 microns in hair shaft diameter on the average, if they are less than 30 then you know there is significant miniaturization.
Hair Loss: Part 2: How does Dr Shapiro treat some of these conditions?
Alopecia in women can be categorized as Female Pattern Hair Loss, alopecia areata, and cicatricial alopecia: lichen planopilaris. In patients with Female Pattern Hair Loss, this is a crucial time to utilize the Ludwig Classification for FPHL.

Female Pattern Hair Loss
When assessing women with Female Pattern Hair Loss, it is important to test for any signs or symptoms of androgen excess. If there are no signs or symptoms, you can determine the class of hair loss based on the Ludwig stage. If there are signs or symptoms of androgen excess, an endocrine work-up should be performed in order to rule out polycystic ovarian syndrome, some kind of adrenal hyperplasia, or another form of androgen excess. You may want to consider referral to either an endocrinologist or a gynecologist. From there, you can assess the Ludwig stage.
If the patient has Ludwig stage III, a hairpiece could be considered, as that is typically their only option. Prices on hairpieces and wigs can vary so that is an important consideration for patients. If you think that the condition will go away, you can suggest a more inexpensive wig/hairpiece from a department store.
Ludwig stages I or II can be treated with topical minoxidil solution (5%) for one year. Topical minoxidil solution is typically used twice per day; however, there are more and more studies demonstrating that a once a day treatment of minoxidil five percent may be as efficacious as minoxidil two percent bid. Women typically do not like the morning application, so Dr Shapiro will use the 5% solution or foam.
What does Dr Shapiro tell his patients?
Dr Shapiro prefers the solution to the foam because it is more precise. He instructs his patients to make five parts and put five drops in each part and spread it with their fingers afterwards. It should not take more than 90 seconds. If a patient complains that it is taking them a long time, ask them exactly what they are doing.

Prevention is key, there is a 65 percent chance of doing so with five percent minoxidil solution.
If there is no improvement, you may want to add:
- antiandrogen therapy + OCA (if childbearing age)
- Hair transplation if donor area dense
- Hair prosthesis
- Hair cosmetics
When it comes to antiandrogen therapy for women, Dr Shapiro uses a lot of spironolactone. He starts at 50mg twice per day for one to two months and then goes to 100mg twice per day if the patient can tolerate it. He always checks their potassium at baseline, one month, and every three months after that. Dr Shapiro also checks their sodium levels. It is important to check all of their electrolytes. There are reports of dilutional hyponatremia with spironolactone and you can end up in trouble. In the elderly population, be sure to check their kidney function as that can also be affected by spironolactone. Of note, spironolactone is approved for women whereas we don’t have a track record with all of the other antiandrogens.
With regards to Propecia (finasteride), Dr Shapiro always warns female patients that he is unsure of what it could do to the breasts, ovaries or uterus 20 to 30 years down the road. We don’t have the long-term data. We do know that it works. Dr Shapiro will use the 2.5mg per day in women; however, keep in mind that this is a Class X drug and spironolactone is a Class D drug so you must warn patients about pregnancy.
What about oral contraceptives?
The oral contraceptives can be categorized as excellent, very good, good, or bad depending on the estrogen component. Products containing drospirenone and cyproterone acetate (available in Canada and other parts of the world) are excellent choices. Very good options include those with norgestimate, desogesterol, and norethindrone acetate. Don’t stop them, because once you stop and start another you can elicit a telogen effluvium or you can unmask or accelerate their androgenetic alopecia even more. If they are on levonorgesterol (a good option), it’s fine, just leave them on it. Stopping and starting birth control pills can create havoc. Norgesterol and norethindrone are bad progestogens. If a patient is on these, Dr Shapiro will get them off of it and change to something else.
Around six months, it is important to assess patient satisfaction with the current treatment. If they are satisfied, that’s great. If they are not satisfied, you may want to consider hair transplantation if the donor area is dense. One in three women have very poor donor areas and you usually cannot do a hair transplant on them. Dr Shapiro usually does strip harvesting in women, you don’t need to do follicular unit extraction because they usually have long hair and don’t care if they have a scar in the back; if they do, you may have to go to follicular unit extraction. For men, you want to do follicular unit extraction because they usually have short hair. For women, Dr Shapiro will take a strip usually around 15-20cm long and usually 1.3cm in width. You then stitch it up and make holes in the front of the scalp and insert them in the holes.
Alopecia Areata
As dermatologists, we are all familiar with how to diagnose and treat this condition to some extent. For centuries, non-specific crude treatment has been used to treat alopecia areata. In the 1800s, they believed that treatments that irritated the scalp seemed to work. To quote Batemen from 1817 “the more caustic a substance and the application of a blister are often extremely successful” and “ointments of oil of mace, turpentine, mustard and black pepper.” Is what they used much different from what we use now? This is how Dr Shapiro treats alopecia areata…
First of all, he looks at the age of the patient. If they are less than ten years old, he will use minoxidil 5% solution with or without a topical corticosteroid or short contact anthralin. If the patient is over ten years old, then Dr Shapiro will look at the extent of scalp involvement. If there is less than 50 percent involvement, he uses intralesional corticosteroids plus or minus minoxidil 5% solution, plus or minus a topical steroid or short contact antralin. In his practice, Dr Shapiro will use 5mg/cc of triamcinolone acetonide and a maximum of 20mg triamcinolone acetonide per month. He feels that is safe and has never had any problems over the last 25 years. If a patient has a large area to be injected, he will go down to 2.5mg/cc and there didn’t seem to be much of a difference. If you have to do the whole scalp, he will use 25mg/cc for a total of 8ccs and he will do 80 injections.
What about topical corticosteroids? A study of 28 patients demonstrated that clobetasol propionate 0.05% under occlusion was effective for the treatment of alopecia totalis/universalis. Dr Shapiro began using clobetasol on his patients and there was a difference regarding hair regrowth. Anthralin one percent for one-hour daily (many times combined with five percent minoxidil) has also shown to be efficacious.
When someone has more than 50 percent of scalp involvement, Dr Shapiro uses contact immunotherapy. He usually uses DPCP and achieves a 78 percent response rate in non-totalis/universalis, but a 17 percent response rate in totalis/universalis. There is a high relapse rate of 62 percent and only half of these patients respond to therapy. Dr Shapiro has bottles in various concentrations and sensitizes not on the arm, but on the scalp. He then applies two coats on half of the scalp initially on the anteroposterior direction, then in the lateral direction, again only on half of the scalp. Make sure that you protect yourself when it is applied because this is extremely immunogenic.
Remember that there is no cure for alopecia areata. Sometimes certain areas do not respond and you may have to combine treatments, just like in psoriasis when you may use polytherapy. Dr Shapiro will inject the areas that are not responding once a month with triamcinolone acetonide and in three out of four weeks they will get the DPCP or dyphencyprone. Dr Shapiro will do the eyebrows as well if he sees that it has worked on the scalp. Problems with this include eczema, blisters, and marked edema. Make sure that your institution will cover you in the event that there are any problems as this is not FDA-approved. Patients need to sign an informed consent. Lymph node enlargement can also occur and the safety of this is unknown; however, Dr Shapiro has never had a case of lymphoma in over 20 years. The only case of lymphoma that he ever had from alopecia areata was a patient who was on cyclosporine. When you are dealing with dark-skinned individuals, be careful with hypopigmentation. NEVER give this to a patient to take home.
If people respond, then the treatment is continued. If they don’t respond, you can consider minoxidil 5 percent solution plus or minus a topical corticosteroid or short contact anthralin, and PUVA. Methotrexate has demonstrated some efficacy at a dose of 20-25mg per week. Dr Shapiro will use 25mg per week for six months and has seen some benefit in patients, especially for the eyebrows.
Lichen Planopilaris
There are different types of lichen planopilaris, i.e., classic lichen planopilaris and frontal fibrosing alopecia. Most dermatologists are only familiar with the classical type and when we look at it under trichoscopy we can see sometimes many hairs coming up out of one hole. We are starting to see more and more of frontal fibrosing alopecia, in fact, Dr Shapiro sees at least two or three new cases per day. It usually occurs in post-menopausal women; however, he has seen it in young women as well, the youngest case being in an eighteen year-old. These patients will start to lose their eyebrows, the hairline will start to recede, and it can also go around the whole scalp.
How do we treat these individuals?
This is all based on experience, as there is no evidence. Dr Shapiro classifies the patients based upon the extent of the condition. If it is less than ten percent hair loss, then he will use clobetasol lotion plus injections with triamcinolone acetonide 10mg/cc for a total of 2ccs. If he sees improvement, he will continue with prn. If there is no improvement, he will treat the patient as if they had more than ten percent hair loss utilizing doxycycline 100mg two times per day or hydroxychloroquine 200mg two times per day, plus or minus ultra-potent topical steroids, plus or minus the injections. Dr Shapiro may also bridge things with prednisone 40mg per day over eight weeks. If there is improvement, he will taper to the lowest effective dose and if there is no improvement there are other options to consider. These options include topical tacrolimus, cyclosprorin A, griseofulvin, mychophenolate mofetil, low-dose isotretinoin, or alefacept.
It has been suggested that these individuals have low PPAR gamma in the scalp. Actos®, a PPAR gamma, did help with symptoms; however, there is an FDA black box warning for bladder carcinoma. This is worrisome for clinicians; however, many of the patients want the treatment. If the patient is aware of the warning and wants the product, Dr Shapiro will give 15-30mg per day.
Take-home Message
When it comes to cicotricial alopecia, they are trichologic emergencies. Early intervention can potentially avert scarring and secondary complications. The diagnosis must be made with a biopsy. Remember that disease-directed medical therapy is only indicated in those with active disease. Adjunctive agents, such as topical minoxidil and hair transplantation, can improve cosmesis.
Trichotillomania
There is a new medication, N-acetyl-cysteine, that has shown a decrease in obsessive compulsive behavior in patients who take 1200-2400 mgs per day. There are hardly any side effects and it can be found in any healthcare store.
In conclusion, it is important to remember that patient education is crucial. There are websites available such as www.carfintl.org, www.naaf.org and www.nahrs.org.
MauiDerm News Editor: Judy Seraphine