The Future of Laser Dermatology
Rox Anderson, MD
Dr Anderson, a professor at Harvard Medical School in Boston, provides us with his views on the future of lasers in dermatology. A lot what the future holds for us is going to be driven by different motivators. Economic change, both globally and nationally, is one of these factors. Dr Anderson feels that we have an obligation, not only for society and our patients, but also to ourselves. Similar care at a higher cost is no longer going to be tolerated. The current generation of dermatologists must embrace and take control of who “extends” them, and how. We have to focus on simplicity, access, efficiency, the idea of being consumer-friendly, and new technology such as apps and social media/crowd-sourcing. We need to be able to provide more for our patients, but we also need to be better and cheaper. What are our “sacred cows?” Who will pay? Who will take the hit? We have to look at what we’re doing and stand back to see how we can be doing it differently.
Dr Anderson predicts a dozen big changes in the field by 2025:
- Smarter lasers that can help reduce risk and monitor skin pigmentation
- Fully software-programmable laser targeting
- A cadre of prescription home-use smart laser, IPL, US devices—all we have right now is basically the hair removal devices
- Melasma will be figured out à specific, effective topical therapy
- Same-day laser tattoo removal, reliably, without scarring
- Useful live microscopy (the real question is, who will read it? what are they used for?)
- Microbiopsies à rapid tissue diagnostics without the pathologist
- “Mohs for Schmohs” –if you can accept the idea that you can have microscopically-guided laser surgery, this will be a video game that the millennials will love playing
- Smart-phone dermatology apps: from ~2000 now to ~200,000
- Excellent, automated melanoma detectors where they belong
- Acne will, in essence, be cured
- Devices that “target” sebaceous glands, ala hair removal
- Sebum inhibitors other than retinoids: PDT, new drugs
- Sunscreens that never wash off
Acne
The one thing that oral retinoids have going for them is that they are the only medicine we have that have a potent suppression of sebum, i.e., sebaceous gland function. What about other ways to do that? If you look at the microanatomy of skin, it is just another part of the hair follicle and Dr Anderson believes that there are many other strategies that can be used to do selective injury to those glands.
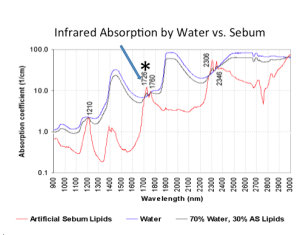
If you look at the absorption spectrum of sebum, at 1726 nm the sebum has a little more absorption than water. This has to do with its lipid content. Dr Anderson and his colleagues used a giant, free electron laser to conduct an experiment at that wavelength testing this hypothesis—whether sebaceous glands can be selectively injured with photothermolysis. The answer is yes. (Sakamoto FH, et al. Selective photothermolysis to target sebaceous glands: theoretical estimation of parameters and preliminary results using a free electron laser. Lasers Surg Med. 2012; 44(2):175-83,) Dr Anderson has a high-powered benchtop prototype 1726 nm laser in the lab specifically designed to go after sebaceous glands…stay tuned.
Sebaceous cryolysis—cold-induced selective injury, could this apply to sebaceous glands in the same way it has been used for fat removal? We know that the sebaceous glands are loaded with lipids, just like fat. At the Wellman Center for Photomedicine (an MGH research center directed by Dr. Anderson) Drs. H.Ray Jalian and Joshua Tam and Conor Evans have been studying the biologic consequences to the sebaceous gland of controlled cold cycles. We see the same things that go on in adipocytes, and actually it’s much easier to trigger because the glands are more superficial.
Dr Anderson feels that we will end up with a cold-induced treatment for acne.
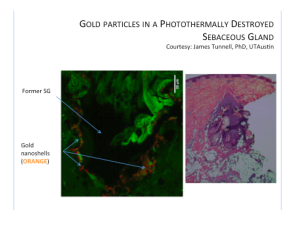
Another strategy for acne would be to put something in the gland that absorbs light. One of the issues with acne drugs is that they are tough to get into the gland. The idea here is to apply something topically, force it into the sebaceous gland, and “fry” it with a pulse of light. In one study, core-shell microparticles worked the best. If you take a nanoparticle and make it out of either silver of gold, plasmon resonance occurs. Silver and gold are both noble metals that have very high conduction so the electrons in them are very free to move. We have an incoming optical field and at the right frequency it is in resonance with the conduction band electrons providing a tremendous amount of energy. You can also design the particles to have their own absorption.
Acne Treatment With Gold-coated Particles
- Clean skin
- Apply particles topically
- Massage to deliver them into follicle
- Remove residual from skin surface
- Treat with laser at the absorption peak wavelength, combined with skin surface cooling
Does this work? Yes, it does.
Using two-photon microscopy in a collaboration with James Tunnell (UT Austin), it was shown that gold particles can be forced into sebaceous glands. After exposure to an 800 nm diode laser, one can see local destruction of sebaceous glands.
Microscopy and Smart Lasers
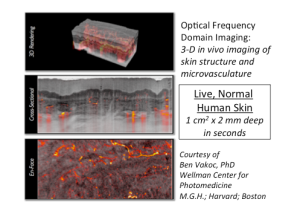
Optical coherence tomography is a means of microscopic imaging. It is fully deployed in ophthalmology and has been for over a decade. In dermatology, it’s used mostly as a research tool.
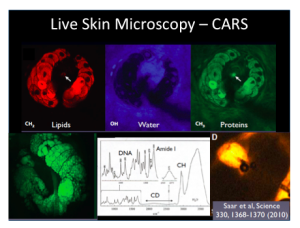
You can see beautiful structure—epidermis, sweat ducts, vasculature, etc. but this hasn’t made its way into clinical practice. If you look further into advanced laser microscopy, we can do some very interesting things. Coherent anti-Stokes Raman scattering (CARS) microscopy requires no stains. It’s a way of setting up a laser microscope that excites the vibrational modes of bonds in various molecules. The bonds are quite specific to the molecule, so you can look at molecular species in the skin. You can tune this process to look at DNA, protein, and lipids. Of great interest, if you replace hydrogen with deuterium, the carbon-deuterium bond is in a very quiet region of the spectrum. You can label drugs with deuterium quite easily and it’s non-toxic. The picture on the bottom right is the first picture that Dr Anderson has ever seen of directly imaging a drug uptake into human skin in a living state. This was performed by tracking deuterium as a label.
The lipid imaging by CARS also gives us beautiful pictures of sebaceous glands. The image above shows sebaceous glands in living mouse skin.
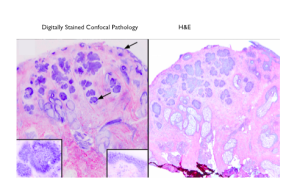
Another major advance, would be to have in vivo microscopes that yield images similar to the familiar H&E staining of conventional histopathology. Dr Daniel Gareau at the Rockefeller Institute has been doing work with digitally stained confocal microscopy. (D.S. Gareau, J. Biomed. Opt. 2009.14(3).)
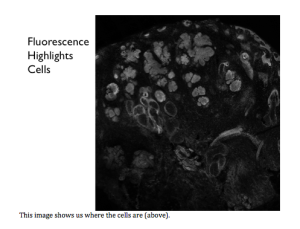
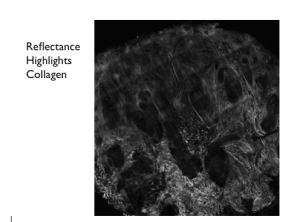
If you look at the reflectance, it shows you where the fibers of collagen are. By staining the fluorescence and the reflectance different colors and putting them together, it gives us something that we, as dermatologists, have all been trained to look at. We are going to see his technique, along with other ones, being melded into a user-friendly version. This entire process takes three minutes and doesn’t require any technicians.
Eulerian Imaging
Remember that except at absolute zero, everything moves. The minor, small motions are not visible; therefore, we think things are stationary. Professor Bill Freeman (MIT) has recently developed Eulerian imaging. It detects small changes in position or color, amplifies them then adds them back onto the original video image. Skin hemodynamics can be revealed in detail, using nothing more than your smart phone. Dr Anderson believes that we may see apps in the future for dynamic oxygen saturation, apps for motile cells, and apps where we can measure the rate of cancer growth. To view Eulerien imaging of the skin, visit: http://www.youtube.com/watch?feature=player_embedded&v=e9ASH8IBJ2U
A New Sunscreen that even Dr Anderson will Use!
There is a new sunscreen under development in collaboration with MIT, Harvard/MGH, and Living Proof. This sunscreen is wearable, breathable, invisible, elastic, and lasts all day. This was first used cosmetically, but it turns out that this film has other properties. What’s interesting is that this film has an SPF of 15 and can be worn for days.
Things That Sound Impossible Now, by 2050:
- Real rejuvenation
- Skin as a user interface
- Synthesis &/or release of drugs or proteins on demand
- Activable implants: particles, designer cells, machines
- Biosensing tattoos and other monitors
- Light-emitting skin
- Hybrid skin: mixing it up with other organs
- Magic Wands
The Magic Wand Project
Every year, Dr Anderson makes just one New Year’s resolution. His 2013 resolution was to somehow empower the young clinicians to actually lead research. Using a 3-D printer, Dr Anderson made some magic wands and gave one to each of the young dermatologists in his department. His instructions were that anytime he/she faced a problem in clinical practice that couldn’t be solved, point the wand at the problem and write it down. Most clinicians do not reflect upon the unique potential that they have, to motivate biomedical research. No one else understands the problems the way that clinicians do. You can’t really define the problem unless you really understand it. Among the clinicians at Mass General, they used the magic wand for one month in practice and generated a list of about thirty practical problems in dermatology that are worth solving. Out of the thirty problems, eight active research projects are underway; each led by a clinical dermatologist.
- Reliable diagnosis of cellulitis
- The world’s best ever sunscreen
- A much better treatment for warts
- Long-lasting blockade of itch and pain
- A great treatment for onychomycosis
- Correction of field cancerization
- Medical grade, personalized cosmetics
- KS / HHV-8 diagnosis in Africa
One of the challenges that we face is to bridge the gap between clinical practice and scientific research. Dr. Anderson enjoys trying to do that.
MauiDerm News Editor-Judy Seraphine