Pediatric Dermatology: What we’ve learned that has changed the way we think about and practice medicine
Sheila Friedlander, MD and Ilona Frieden, MD
Part 1: Look What the Wind May Have Blown In
Dr Friedlander began this session with a case study….A child presents to your office with an unusual rash. The pediatrician called it maculopapular, others migth call it polymorphous. The rash is papular , erythematous and fairly generalized. Dr Friedlander states that most of the time when a child comes into your office with this type of rash, the history is often not that helpful. Be sure to ask about systemic signs, fever, or anyone else sick in the house. Obtain a drug exposure history. . What is it reasonable to think about? Most of the time, it is a virus. Enterovirus is a reasonable possibility When in doubt, some physicians will blame EBV, especially if the child has had amoxicillin. Occasionally, it could even be measles with this sort of polymorphous eruption, so it is important to look for cough, coryza, and conjunctivitis. It could also be Parvo virus so check to see if the child had “slapped cheeks” appearance at any point, or a lace-like appearance to the body rash. . This particular child has had high fevers for four days and the family is starting to get anxious. The patient is fussy and his lips are cracked. The parents also inform you that the child took amoxicillin two days ago and some NSAIDs yesterday. What do you think this is? Dr Friedlander again emphasizes that it is important to go through his history of drug exposure; fortunately in this case, the rash predates any medications.
When you examine the eyes, you note the conjunctiva are red with a rim or halo of white around the cornea,, which is called limbal sparing—In the diaper area, there is superficial desquamation that is really faint superimposed on confluent erythema. . What can cause superficial desquamation in this pattern. What about staph scalded skin? The kids who have staph scalded skin do have intertriginous area involvement, but also often have erythema in the perioral and periorbital areas along with radiating fissures around the mouth. They may also have blisters or bullae.
When you see a patient like this, you need to think about virus, drug, and staph scalded skin. Remember, this child has a polymorphous rash, has lip and tongue involvement, and a very distinctive diaper-area rash that developed early in his course. The child also has conjunctivitis with limbal sparing and one enlarged lymph node.
So, what should we be thinking about? Kawasaki Disease…Dr Friedlander reminds us to consider this whenever we see a child who has had prolonged fever and a rash.
A 2013 article by Bayers S, et al was published in the JAAD, and is an extremely useful review for dermatologists interested in Kawasaki Disease. This disease is a small and medium size artery vasculitis. One of the diagnostic criteria is fever for more than five days; however, if you have a child that fits all of the criteria at day four, you should move ahead with treatment. The earlier you start intervention, the less likely the child is to develop coronary artery disease. The palms and soles are often red and swollen, and the aforementioned findings of conjunctival injection along with crusted lips and oral mucous membrane erythema are often present. Cervical l adenopathy is often present but usually asymmetrical—this is helpful to remember. If you suspect Kawasaki disease, get an expert in the area to help you manage this patient.
What are other KD skin findings that are of interest to dermatologists?
- Micropustular follicular rash (uncommon)
- Nail discoloration, onychomadesis
- BCG site rash
- New onset psoriasis
Kawasaki Disease: Epidemiology
The typical age at presentation is six months to five years of age and the highest incidence of the disease is in Asian countries. In the United States, the highest incidence is among those of Asian ethnicity. If a child has this disease, the risk for a sibling to develop the disease is six to 30 times higher than normal and for any progeny of KD patients, , the risk for his/her child is two times higher. The recurrence rate is two to four percent.
Why is this disease so important? Coronary artery aneurysms and cardiac disease!
It is extremely important to make the diagnosis because cardiac complications can occur. These include:
- Coronary ectasia and aneurysms
- Decreased coronary arterial compliance
- Myopericarditis
- Arrhythmias
- Ischemic heart disease
- Pericardial effusion
- Valvular regurgitation
- Myocardial infarction
- Sudden cardiac death
Cardiac complications affect 15 to 25 percent of untreated patients.
Treatment for Kawasaki Disease
Again, refer to a specialist to help manage these patients. Treatment can decrease coronary risk by at least a factor of five. Treatment includes IVIG 2gram/kilogram over 12 hours, ASA High (80-100mg) divided qid, then low-dose (3-5mg) around day 14. Corticosteroids may be useful in refractory patients. Biologics, such as infliximab and etanercept, may also be useful. IVIG should be repeated if there is no defervescence at 36 hours.
What causes this disease?
We know that cases tend to occur close to each other temporally and there is a prediliction for winter and spring. It occurs mostly in children and is self-limiting. It takes a course similar to that of infectious processes where immune-mediated response is apparent. Lots of organisms have been implicated; yet the etiology remains elusive..
Over the last few years, researchers have found that a correlation exists between wind currents that track from Asia to Japan which traverse the North Pacific and the occurrence of Kawasaki disease. There have been three epidemics in Japan in May, March, and April, which correlate with times of highest intensity wind currents The belief is that there may be a wind-borne environmental trigger. Investigators are now utilizing planes and are collecting samples of air in the middle of these wind currents. Many scientists believe that there is a wind-borne agent that is causing this disease. Stay tuned, we may have more information next year.
Part 2: What is a Birthmark?
In the broad sense, a birthmark is a developmental anomaly that is present on the skin. As you know, they do not necessarily need to be present on the day of birth and they can range from common to rare.
Dr Frieden discusses the six questions that you should ask when you see a child with a birthmark.
- What is the diagnosis? Is this a port wine stain or is this a premonitory mark of an infantile hemangioma. It is extremely important to pin down the diagnosis.
- Is there a risk of extracutaneous associations?
- What is the prognosis/natural history?
- What (if anything) needs to be done? Are there good treatments?
- Is there a “window of opportunity?”—an example of this would be infantile hemangioma whereby early intervention can really make a difference if treatment is needed
- What is the cause?
Dr Frieden has been a pediatric dermatologist for a little over thirty years and she states that parents always ask: “what caused this?” Previously, the answer was “we don’t know”. Often times, especially for mothers, they ask themselves if they did something wrong during the pregnancy.
So to answer the sixth question, according to Dr Frieden, “2013 has really been a watershed year.” Researchers are now using deep sequencing of birthmark tissue, not germ-line DNA in order to understand the genes that cause birthmarks. Most of the birthmarks that appear are post-zygotic somatic mutations. Knowing the cause of the birthmark may help to pave the way for newer therapies.
In 2013 Mutations In….
- GNAQ cause Sturge-Weber
- KRAS and HRAS causes of nevus sebaceous
- NRAS cause of giant nevi
- GTPase BMS1 cause of familial aplasia cutis congenital (germ-line)
What’s exciting about this? New therapies will be developed to address activating mutations because these are also mutations that can cause cancer. We know that researchers are looking for ways to stop activating mutations in these pathways. So you may ask “how does this affect a birthmark?” Dr Frieden provides an example where it may be very important and that is in Sturge-Weber. In Sturge-Weber, children are generally born with Sturge-Weber and they are neurologically normal, there are exceptions to this; however, Sturge-Weber is really a progressive disease. Children will develop heavy paralysis and seizure disorder despite the fact that they are normal at birth. It may be that if we treated these patients with something that inhibited an activated mutation GNAQ only for a couple of years, for example, we may be able to avoid some of the developmental changes that occur. Scientists don’t really know whether or not this is true, but it is an example of where we may be able to halt progression. This is an incredibly exciting time because, as physicians, we may be able to look parents in the eye and provide them with some information about the cause of the birthmark.
Part 3: Drug Reactions in Kids
This section of the presentation focused on drug reactions.,foc. Why is Dr Friedlander cautious when prescribing minocycline? There is more and more evidence that minocycline is one of the offenders that can cause Drug Reaction Eosinophila and Hypersensitivity Syndrome (DRESS). It’s important to be aware of this disorder and how frequently we can see it. It can occur in one in 1,000 to 10,000 drug exposures. DRESS can be distinguished from other drug reactions in that often times the onset is later, approximately two to six weeks after exposure. It presents with a morbilliform rash, significant facial and periorbital edema, and exfoliative changes. Why is it of concernt? DRESS can affect the liver and other organs and has a mortality rate of up to ten percent. This is a good discussion to follow in that of Kawasaki Disease because they share a similar differential diagnosis. Patients with DRESS have bilateral, significant cervical adenopathy, there may also be significant facial edema, and often have what looks like an extensive erythematous, sometimes edematous, confluent eruption. Husain Z, et al published a very useful review in the JAAD in 2013 regarding clinical perspectives and management and therapeutics for DRESS syndrome.
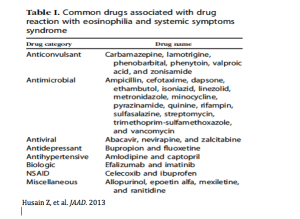
What are the drugs that we need to worry about?
When considering DRESS, you want to check to see if the patient has eosinophilia and/or liver involvement because such findings raise the likelihood of life-threatening complications. . The common drugs associated with this problem are outlined below:
Pathogenesis
We now know that there are some genetic polymorphisms for drug metabolism that DRESS patients may exhibit. For many of these patients, there may be a genetic difference in how these drugs are metabolized which may be a cause of the disease. There are two enzymes that have been implicated, epoxide hydroxylase and glutathione transferase. Another fascinating discovery is the association between DRESS and human herpes virus (HHV-6), CMV, or EBV. Researchers are really not sure whether or not this a secondary involvement, but some scientists feel that re-activation may play an important role. In fact, there are some studies that have demonstrated that those who receive amoxicillin are worse prognostically because amoxicillin, at least in vitro, can help encourage activation and replication of HHV-6. This is an interesting combination of environmental and immune reactions. A number of specific genetic markers have been identified: these include HLA-A 3101 in association with carbamazapine; HLAB-5801 with allopurinol; and HLA DR3 and HLADQ2 with carbamazapine that put certain patients at risk.
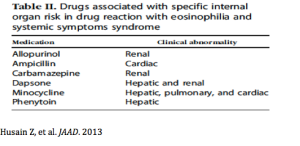
What organ is likely to be involved if your patient gets DRESS?
Don’t forget to think about the differential diagnosis. Remember that the interval before onset is longer than Stevens Johnson Syndrome and TEN. Organ involvement is also more common in DRESS. These patients also tend to have more facial swelling and symmetrical nodes as opposed to Kawasaki Disease. If you were to perform a biopsy in these patients, you would see a more predominant lymphocytic infiltration whereas in Stevens Johnson Syndrome or TEN you would see a predominance of necrosis.
What can you do if you think your patient has had a reaction to DRESS?
First and foremost, you want to discontinue the drug. . You can also do skin or serum testing; this provides a positive predictive value; however, it is not widely used. Therapy for DRESS includes supportive care, systemic l corticosteroids if there is liver involvement, and avoiding the use of antibiotics or NSAIDs.
Prednisone 1mg/kg/day is often utilized, and tapered slowly over three to six months. If there is no response, patients can be given IV methylprednisolone 30mg/kg IV qd for three days. Do not stop these kids abruptly as there relapse can occur. It is also very important to check thyroid function.
Dysphagia
Some experts believe that ysphagia is an early manifestation of DRESS syndrome and it may come before the rash. Why is this important? Many times children will present to the pediatrician with a sore throat and will be given amoxicillin empirically. With the advent of rapid Strep tests, Dr Friedlander would encourage all pediatricians to utilize these tests before simply prescribing amoxicillin, as we know that there is a suggestion that it may be detrimental to patients with evolving DRESS.. Dr Friedlander also recommends antipyretics with Tylenol versus NSAIDs. Remember to ask if the patient is feeling uncomfortable or having trouble swallowing.
MauiDerm News Editor-Judy Seraphine