Whitney J. High, MD, JD, MEng
- Dermatopathology is one of two ABMS-recognized subspecialties in dermatology, and one may become fellowship trained after first being a board-certified dermatogist or general pathologist.
- Biopsy use is increasing. In nine geographic areas of the USA, over the time period 1986-2001, the biopsy rate among those >65 years of age rose 2.5-fold, and the melanoma rate rose 2.4-fold.
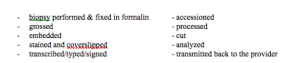
- There are multiple steps involved in taking a specimen from a piece of “wet” tissue, in formalin, to an interpretable slide and to a typewritten report. These steps include:
- The dermatopathologist is examining but a small portion of your original sampling, and this must always be considered when one assesses the “representative nature” of the results.
- There is an old mantra in pathology in general: crap in = crap out. No dermatopathologist, regardless of skill or expertise, can weave a poor sampling into an outstanding result.
- It is the clinician responsibility to secure a “representative biopsy”, and if this is not done, eventually, this inadequacy will be discovered. Over the period of 1998-2005 the number of shaves increased but the volume of shaves decreased.
- The technique employed (shave, punch, excision) must be adapted to the clinical situation – there are no fixed rules that may be applied to every situation. This is why the clinician is being paid an “evaluation/management” code; namely, to select a biopsy that is appropriate for the circumstances.
- A recent study of pigmented lesions showed the odds of misdiagnosis (overall and associated with an adverse outcome) were much higher with a punch biopsy than with an excisional biopsy, whereas a shave biopsy was only weakly associated with misdiagnosis. (Ng et al. 2010)
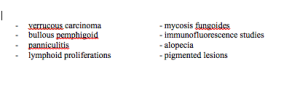
- Situations where the biopsy technique should be carefully considered include suspected:
- The pathology report itself should be carefully read and scrutinized to understand precisely what the dermatopathologist is trying to convey. Demographic data should be confirmed. The technique and specimen size should be verified. Data used by the dermatopathologist to formulate the diagnosis should be noted (i.e., step levels, immunostains, special stains, etc.). If questions still exist, a phone call should be placed to the dermatopathologist for expanded dialog.