Update on Psoriasis Comorbidities
Joel M. Gelfand, MD, MSCE
Dr Joel Gelfand provides us with an update on the comorbidities often associated with psoriasis. Over the last decade, we have been able to identify factors that may contribute to comorbidities in psoriasis. Environmental risk factors include smoking and obesity. Scientists have also identified genes and loci associated with psoriasis, diabetes, and cardiovascular disease including PSORS2/3/4, CDKAL1, ApoE4, and TNFAIP32. We should also consider mediating factors such as pathophysiology, effects of treatment, and the psychosocial impact of psoriasis. (Azfar RS, Gelfand JM. Curr Opin Rheum 2008;20:416–422)
Currently, data suggest that we do have well-established comorbidities of psoriasis. These include:
- Heart attack, stroke, cardiovascular death
- Metabolic syndrome
- Diabetes
- Psoriatic arthritis
- Mood disorders (anxiety, depression, suicide)
- Crohn’s disease
- T cell lymphoma (rare)
The risk of cardiometabolic disease in patients appears to increase with more severe disease. What does this mean clinically? As previously noted, patients with more severe psoriasis experience an increased risk of MI, stroke, cardiovascular death, and diabetes. There is an average of five years of life lost. The ten-year risk of a major CV event attributable to psoriasis is six percent. Literature suggests that the risk of cardiovascular disease in patients with severe psoriasis is comparable to the risk conferred by diabetes. Additionally, patients treated for severe psoriasis are 30 times more likely to experience MACE (attributable to psoriasis) than to develop a melanoma.
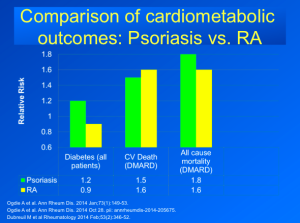
Research has also been conducted using UK-based data comparing cardiometabolic events in psoriasis versus rheumatoid arthritis (RA). We can see that patients with psoriasis have a higher rate of diabetes, but this is not seen with RA patients. There is something specific about psoriatic disease making one more prone to developing diabetes over time. (See Figure 1) These data also demonstrate that psoriasis patients treated with systemic or phototherapy have a similar increased risk of CV and all cause mortality compared to RA treated with disease modifying treatments.
FIGURE 1
Clinicians should recognize that metabolic problems start early and there is emerging pediatric data. The prevalence of the metabolic syndrome in pediatric psoriasis is 30 percent versus 7.4 percent in the control population.
The skin of patients with psoriasis has increased regulation/expression of cardiometabolic genes, more so than the up-regulation of inflammatory genes. This tells us that the skin itself may be the source of the abnormalities that we’re seeing.
We should also remember that psoriasis is more than just skin deep. Psoriasis is associated with increased vascular inflammation independent of traditional risk factors and equivalent to ten years of aging. Advanced FDG-PET/CT imaging demonstrated subclinical inflammation in the liver and joints.
How are we doing as healthcare providers?
Overall, cardiovascular risk factors are under-screened and under-managed in patients with psoriasis. CDC US population data indicates poor screening rates for hypertension—only four percent of severe psoriasis patients receive screening for hypertension in the dermatology office versus 61 percent patients in the non-dermatology setting.
Should we treat psoriasis aggressively to lower the risk of CV disease?
The answer is that we really don’t know for certain. Observational data suggest that methotrexate and TNF inhibitors lower the risk of cardiovascular events. Data do not yet exist to determine a protective effect of phototherapy, apremilast, and ustekinumab on CV events. (Micha R et al. Am J Cardiol 2011;108:1362–1370; Barnabe C et al. Arthritis Care Res (Hoboken) 2011;63:522–529; Prodanovich S et al. J Am Acad Dermatol 2005;52:262–267; Wu JJ et al. Arch Dermatol 2012;148:1244–1250; Ahlehoff O et al. J Int Med 2013;273:197–204)
Emerging Comorbidities
Newer data suggest that following are also comorbid conditions associated with psoriasis:
- Sleep apnea
- Nonalcoholic steatohepatitis (NASH)
- Chronic obstructive pulmonary disease (COPD)
- Adverse infectious disease outcomes
- Chronic and end-stage renal disease
- Peptic ulcer disease
Moderate to severe psoriasis is also a risk factor for chronic kidney disease (CKD). Data suggest that there is nearly a two-fold risk of moderate to advanced CKD among psoriasis patients and a greater than four-fold risk of end stage renal disease requiring dialysis. Risks are independent of diabetes, hypertension, and nephrotoxic medication. The risk of CKD associated psoriasis is greater than the risk of CKD associated with diabetes and hypertension. (Wan J, Wang S, Denburg MR, Shin DB, Gelfand JM. Risk of moderate to advanced kidney disease in patients with psoriasis. BMJ 2013;15;347:f5961)
There are clear clinical implications that comprehensive care is required for patients with psoriasis as we shift from the old paradigm of “just a skin disease” to the new paradigm of “a systemic disease.”
Clinical Implications
Standard Screening Recommendations (US Preventative Services Task Force (HTN) 2007; American Diabetes Association Guidelines 2014 (Diabetes Care 2014;37:S5-S13); ACC/AHA 2013 Guideline on the assessment of CV risk)
- Hypertension
- Every 2 year if BP <120/80 mm Hg
- Every year if BP 120 to 139/80 to 89 mm Hg.
- Diabetes (Fasting plasma glucose, HbA1c, or OGTT)
- Adults ≥ 45
- Adults BMI ≥25kg/m2 who have one or more additional RFs
- Repeat every 3 years
- Cardiovascular risk assessment:
- Traditional risk factors every 4-6 years in patients 20-79
- Estimate 10 year risk in those 40 -79
Psoriasis and Cancer
We should remember to encourage patients to stay up-to-date on age appropriate cancer screenings, including cervical cancer, colon cancer, breast cancer, and lung cancer. (CDC guidance accessed 1/21/14Note: Earlier Screening recommended in those at high risk; Moyer VA et al Screening for lung cancer: US Preventative Services Task Force recommendation statement. Ann Internal Med. doi:10.7326/M13-2771)
- Cervical cancer: Pap smear (q 2-3 yrs ages 21-65)
- Breast cancer: mammography (50-74, q 2 yrs)
- Colon cancer: (50-75) fecal occult blood q year, flex sig q5 yrs, colonoscopy q10 yrs)
- Lung cancer: Annual low dose CT screening for 55-80 with ≥30 pack year history and current smoker or quit within 15 years
Large, long-term follow-up studies are necessary to determine the risk of cancer with psoriasis treatments.
Psoriasis and Infection
It is important that we screen psoriasis patients for streptococcal infection with guttate flares. In severe psoriasis, it’s also important to test for HIV. Psoriasis patients who are undergoing immune suppressive treatments should stay up-to-date with all recommended vaccinations as well, including influenza, pneumonia, zoster, hepatitis B, and HPV. (http://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf)
Psoriasis and Mood Disorders
Healthcare providers should ask patients about depression and anxiety symptoms and monitor the impact of treatment on psychiatric symptoms as well as refer for treatment when appropriate. Some data suggest that cognitive behavioral therapies and meditation may modestly enhance the response to psoriasis treatment.
Psoriasis and PsA
Remember the importance of identifying the signs and symptoms of psoriatic arthritis, including:
- Morning joint stiffness
- Joint pain that improves with activity
- Swollen, tender joints, dactylitis, enthesitis
- Check X rays of affected joints and CRP
- Co-manage with rheumatology, DMARDs
In conclusion, we have to look beyond the skin for our psoriasis patients. A comprehensive care approach is essential for our patients. Patients should be educated about the disease, treatment, and associated risk factors.